Cytotoxic effects of three different oral antiseptic solutions on epithelial cells of buccal mucosa
Abstract
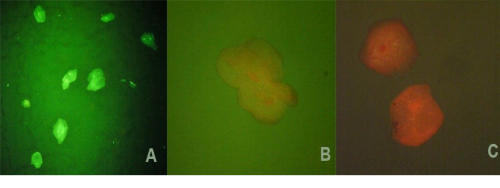
There is a great number of different oral antiseptic solutions on the market. The effects of antiseptic solutions reflect in number of bacteria reduction, antiplaque effect, anti-inflammatory and anti-cariogenic effects and also in eliminating halitosis. In numerous studies that tested antimicrobial effect of different antiseptic solutions, it was found that all solutions have certain antimicrobial effect that is particularly expressed in solutions with octenidine and chlorhexidine. There are few data on cytotoxicity of antiseptics on keratinocytes of buccal mucosa. Aim of this study was to test and compare cytotoxic effects of three different commercial oral antiseptic solutions on keratinocytes from smear of buccal mucosa. Pilot experimental study. Solutions used in the study are: Hibidex DAP* 0.12%, Ozоsept* and Octenisept* sprays. Smears were taken from buccal mucosa of six healthy volunteers. The study was designed by using 90% antiseptic solution with cells. Cytotoxic effect of antiseptic solution on cells was measured after one, three, five, ten, fifteen, twenty, twenty five and thirty minutes by preparing sample with cells that were in antiseptic solution. The samples were stained with acridine orange/ethidium bromide (AO/EB), and observed under a fluorescence microscope. The cytotoxic effect was expressed in percentage of live cells. Testing cytotoxicity of oral antiseptic solutions Hibidex DAP*, Octenisept* and Ozosept* has showed that the viability of keratinocytes taken from the buccal mucous membranes which are under the influence of the solutions, decreases progressively in time. We noticed that the cytotoxic effects of some solutions manifested gradually, while the transitional forms of viability had not been verified when it came to the effect of Hibidex DAP*, because in a very short period of time it showed 100% negative effect on cell viability. Octenisept* and Ozosept* compared to Hibidex DAP*, have a lower level of cytotoxicity of the active ingredient for oral mucosal keratinocytes.
Full Text:
PDFReferences
Marchetti E, Mummolo S, Di Mattia J, Casalena F, Di Martino S, Mattei A et. al. Efficacy of essential oil mouthwash with and without alcohol: a 3-day plaque accumulation model. Trials. 2011 Dec; 15;12:262.
Welk A, Zahedani M, Beyer C, Kramer A, Müller G. Antibacterial and antiplaque efficacy of a commercially available octenidine-containing mouthrinse. Clin Oral Investig. 2016 Sep;20(7):1469-76.
Research, Science and Therapy Committee of the American Academy of Periodontology. Treatment of plaque-induced gingivitis, chronic periodontitis and other clinical conditions. J Periodontol. 2001 Dec;72(12):1790-800.
Parashar A. Mouthwashes and Their Use in Different Oral Conditions Scholars Journal of Dental Sciences (SJDS). 2015;2(2B):186-91.
Cortelli JR, Barbosa MD, Westphal MA. Halitosis: a review of associated factors and therapeutic approach. Braz Oral Res. 2008 Aug;22 Suppl 1:44-54.
Müller G, Kramer A. Biocompatibility index of antiseptic agents by parallel assessment of antimicrobial activity and cellular cytotoxicity. J Antimicrob Chemother. 2008 Mar; 61(6):1281-7.
Uzer Celik E, Tunac AT, Ates M, Sen BH. Antimicrobial activity of different disinfectants against cariogenic microorganisms. Braz Oral Res. 2016 Nov; 28;30(1):e125.
Rohrer N, Widmer AF, Waltimo T, Kulik EM, Weiger R, Filipuzzi-Jenny E, et. al. Antimicrobial efficacy of 3 oral antiseptics containing octenidine, polyhexamethylene biguanide, or Citroxx: can chlorhexidine be replaced? InfectControl Hosp Epidemiol. 2010 Jul;31(7):733-9.
Tirali RE, Bodur H, Sipahi B, Sungurtekin E. Evaluation of the antimicrobial activities of chlorhexidine gluconate, sodium hypochlorite and octenidine hydrochloride in vitro. Aust Endod J. 2013 Apr;39(1):15-8.
Giannelli M, Chellini F, Margheri M, Tonelli P, Tani A. Effect of chlorhexidine digluconate on different cell types: a molecular and ultrastructural investigation. Toxicol In Vitro. 2007 Mar;22(2):308-17.
Balloni S, Locci P, Lumare A, Marinucci L. Cytotoxicity of three commercial mouthrinses on extracellular matrix metabolism and human gingival cell behaviour. Toxicol In Vitro. 2016 Aug;34:88-96.
Schmidt J, Zyba V, Jung K, Rinke S, Haak R, Mausberg RF, Ziebolz D. Cytotoxic effects of octenidine mouth rinse on human fibroblasts and epithelial cells - an in vitro study. Drug Chem Toxicol. 2016 Jan;39(3):322-30.
Flemingson, Emmadi P, Ambalavanan N, Ramakrishnan T, Vijayalakshmi R. Effect of three commercial mouth rinses on cultured human gingival fibroblast: an in vitro study. Indian J Dent Res. 2008 Mar;19(1):29-35.
Tirali RE, Bodur H, Ece G. In vitro antimicrobial activity of sodium hypochlorite, chlorhexidine gluconate and octenidine dihydrochloride in elimination of microorganisms within dentinal tubules of primary and permanent teeth. Med Oral Patol Oral Cir Bucal. 2012 May;17(3):e517-22.
Zelić O, Cakić S, Luković N. The effect of two different oral antiseptics on dental plaque formation (de novo biofilm) and on gingival inflammation. Srp Arh Celok Lek. 2009 Jan-Feb;137(1-2):6-9.
Veldhuizen EJ, Tjeerdsma-van Bokhoven JL, Zweijtzer C, Burt SA, Haagsman HP. Structural requirements for the antimicrobial activity of carvacrol. J Agric Food Chem. 2006 Mar;8;54(5):1874-9.
Tanasković-Stanković S, Cabunac J, Kanjevac T, Milosavljević Z. Differential histomorphometric changes in normal and inflamed gingival epithelium. Sanamed. 2016 Jul;11(3):197-201.
Wanda M, Haschek, Colin G, Rousseaux, Matthew A. Wallig. Skin and Oral Mucosa. Fundamentals of Toxicologic Pathology. 2nd ed. 2010;135–61.
Goldschmidt P, Cogen R, Taubman S. Cytopathologic effects of chlorhexidine on human cells. J Periodontol. 1977 Apr;48(4):212-5.
Refbacks
- There are currently no refbacks.
