Seroprevalence of HEV infection and risk factors among Sudanese pregnant women in Khartoum state
Abstract
Abstract
Background: Hepatitis E virus (HEV), a single-stranded, positive-sense RNA virus is responsible for acute Hepatitis E epidemics in many developing countries. HEV infection in pregnant women is more common and fatal in the third trimester. The incidence of acute viral hepatitis E is known for being the cause of major outbreaks of waterborne hepatitis in Africa. Traditional sanitation and water supplying systems are one of the most important factors for the virus transmission.                                                                                                                  Â
 Objectives: our aims were to confirm the incidence of Hepatitis E virus among pregnant women attending Khartoum teaching hospitals and to detect the association of abortion in women with HEV infection, the relative risk factors and clinical symptoms.
Methods: Ninety-three pregnant women were enrolled in this study. Enzyme linked immunoassay (ELISA) was performed to determine the presence of anti-HEV IgG during the period from March to May 2015.
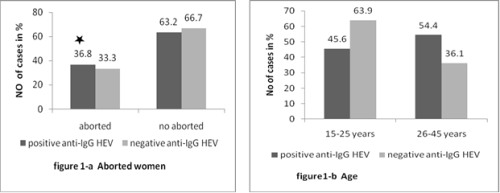
The results: HEV IgG antibodies were detected in 61.2% (57/93) of the women under study. The highest percentages were recorded in third trimesters of pregnancies 62.5% (34/57). HEV is associated with high rates of spontaneous abortion, we found about 36.8% (21/57) of HEV positive patients abortive with odd ratio above 1 which means that HEV is considered as risk factor for abortion among pregnant women. While other risk factors include water system supplies, age groups (26-45), rural residence, history of blood transfusion and travelling out of Sudan were 71.9% (41/54), 54.4% (31/57), 50.9% (29/57), 12.3% (7/57) and 5.3% (3/57) respectively. The symptoms were variable with no significant interpretations.
Conclusion: In this study, we found a high frequency of anti-HEV IgG among Sudanese pregnant women in Khartoum which is endemic in Sudanese habitant original root that had never travelled out of the country. Also the present study indicated that one of the highest risk factor is water hygiene cautions. HEV positive patient's symptoms are not reliable for HEV diagnosis which needs more sensitive and specific diagnostic tools to confirm the result.
Full Text:
PDFReferences
Balayan, M. S., A. G. Andjaparidze, S. S. Savinskaya, E. S. Ketiladze, D. M. Braginsky, A. P. Savinov, and V. F. Poleschuk. Evidence for a virus in non-A, non-B hepatitis transmitted via the fecal-oral route. Intervirology.1983;20:23–31.
Tam, A. W., M. M. Smith, M. E. Guerra, C. C. Huang, D. W. Bradley, K. E. Fry, and G. R. Reyes. Hepatitis E virus (HEV): Molecular cloning and sequencing of the full-length viral genome.Virology.1991;185:120–131.
Okamoto, H. Genetic variability and evolution of hepatitis E virus. Virus Res. 2007; 127:216 --228.
Kantala T, Heinonen M, Oristo S, von Bonsdorff CH, Maunula L. Hepatitis E virus in young pigs in Finland and characterization of the isolated partial genomic sequences of genotype 3 HEV. Foodborne pathogens and disease. 2015;12(3):253-60.
Fu H, Wang L, Zhu Y, Geng J, Li L, Wang X, et al. Analysing complete genome sequence of swine hepatitis E virus (HEV), strain CHN-XJ-SW13 isolated from Xinjiang, China: putative host range, and disease severity determinants in HEV. Infection, genetics and evolution : journal of molecular epidemiology and evolutionary genetics in infectious diseases. 2011;11(3):618-23.
Bihl F, Negro F. [New aspects of HEV infection]. Revue medicale suisse. 2008;4(169):1863-6.
Kluge M, Fleck JD, Soliman MC, Luz RB, Fabres RB, Comerlato J, et al. Human adenovirus (HAdV), human enterovirus (hEV), and genogroup A rotavirus (GARV) in tap water in southern Brazil. Journal of water and health. 2014;12(3):526-32
Blackburn BG, Craun GF, Yoder JS, Hill V, Calderon RL, Chen N, et al. Surveillance for waterborne-disease outbreaks associated with drinking water--United States, 2001-2002. Morbidity and mortality weekly report Surveillance summaries. 2004;53(8):23-45.
Calderon RL, Craun GF. Estimates of endemic waterborne risks from community-intervention studies. Journal of water and health. 2006;4 Suppl 2:89-99.
Shanan S, Abd H, Bayoumi M, Saeed A, Sandstrom G. Prevalence of protozoa species in drinking and environmental water sources in Sudan. BioMed research international. 2015;2015:345619.
Emerson SU, Purcell RH: Hepatitis E virus. Rev Med Virol. 2003; 13:145-154.
Irshad M: Hepatitis E virus: an update on its molecular, clinical and epidemiological characteristics. Intervirol. 1999; 42: 252-262.
Smith DB, Purdy MA, Simmonds P. Genetic variability and the classification of hepatitis E virus. J Virol. 2013;87(8):4161-9.
Patra S, Kumar A, Trivedi SS, Puri M, Sarin SK. Maternal and fetal outcomes in pregnant women with acute hepatitis E virus infection. Ann Intern Med 2007;147(1):28-33.
Devi SG, Kumar A, Kar P, Husain SA, Sharma S. Association of pregnancy outcome with cytokine gene polymorphisms in HEV infection during pregnancy. J Med Virol 2014;86(8):1366-76. Epub 2014 Mar 7.
Fiore S, Savasi V. Treatment of viral hepatitis in pregnancy. Expert Opin Pharmacother 2009;10(17):2801-9.
Navaneethan U, Al Mohajer M, Shata MT. Hepatitis E and pregnancy: understanding the pathogenesis. Liver Int 2008; 28(9):1190-9. Epub 2008 Jul 25.
Ranger-Rogez S, Alain S, Denis F. Hepatitis viruses: mother to child transmission [article in French]. Pathol Biol (Paris) 2002; 50(9):568-75.
Naidu SS, Viswanathan R. Infectious hepatitis in pregnancy during Delhi epidemic. Indian J Med Res 1957;45(Suppl):71-6.
Krain LJ, Atwell JE, Nelson KE, Labrique AB. Fetal and neonatal health consequences of vertically transmitted hepatitis E virus infection. Am J Trop Med Hyg 2014;90(2):365-70. Epub 2014 Jan 13.
Rasheeda CA, Navaneethan U, Jayanthi V. Liver disease in pregnancy and its influence on maternal and fetal mortality: a prospective study from Chennai, Southern India. Eur J Gastroenterol Hepatol 2008;20(4):362-4.
Rayis DA, Jumaa AM, Gasim GI, Karsany MS, Adam I. An outbreak of hepatitis E and high maternal mortality at Port Sudan, Eastern Sudan. Pathog Glob Health 2013;107(2):66-8.
Guthmann, J. P., H. Klovstad, D. Boccia, N. Hamid, L. Pinoges, J. Y. Nizou, M. Tatay, F. Diaz, A. Moren, R. F. Grais, I. Ciglenecki, E. Nicand, and P. J. Guerin. A large outbreak of hepatitis E among a displaced population in Darfur, Sudan.The role of water treatment methods. Clin. Infect. Dis, 2004; 42:1685–1691.
Aggarwal R, Krawczynski K: Hepatitis E: an overview and recent advances in clinical laboratory research. J Gastroenterol Hepatol, 2000; 15:9-20.
Purcell RH, Emerson SU: Hepatitis E: an emerging awareness of an old disease. J Hepatol 2008, 48:494-503.
Benait VS, Sander V, Purikh F, Muragesh M, Ranka VS: Outcome of acute hepatic failure due to acute hepatitis E in pregnant women. Indial J Gastroenterol 2007, 26:6-10.
Boccia D, Guthman JP, Klovstad H, Hamid N, Tatay M, Ciglenecki I, Nizou JY, Nicand E, Guerin PJ: High mortality associated with an outbreak of hepatitis E among displaced persons in Darfur, Sudan. Clin Infect Dis. 2006; 42:1679-1684.
Barnett BJ, Sehulster L. Austin, TX, USA: Disease Prevention News, Texas Department of Health. Hepatitis E: Could it happen here? ; 1996. 56: 1–2.
Zuhal Ahmed Al-Tayeb, Mohammed Nafi and Mustafa EM Yassin. Frequency of Hepatitis E Virus among Pregnant Women Attending Khartoum Hospitals. American Journal of Research Communication, 2014;2(4) :241-247.
Stoszek SK, Abdel-Hamid M, Saleh Doa'a, Kafrawy SE, Narooz S, Hawash Y, Shebl FM, Daly ME, Said A, Purcell RH, Strickland T: High prevalence of hepatitis E antibodies in pregnant Egyptian women. Trans Roy Soc Trop Med Hyg. 2006;100:95-101.
Patra S, Kumar A, Trivedi SS, Puri M, Sarin KS: Maternal and fetal outcomes in pregnant women with acute hepatitis E virus infection. Ann Intern Med. 2007; 147:28-33.
Huang F, Wang J, Yang C, Long F, Li Y, Li L, et al. Chinese pregnant women in their third trimester are more susceptible to HEV infection. The Brazilian journal of infectious diseases : an official publication of the Brazilian Society of Infectious Diseases. 2015;19(6):672-4.
Gad YZ, Mousa N, Shams M, Elewa A. Seroprevalence of subclinical HEV infection in asymptomatic, apparently healthy, pregnant women in Dakahlya Governorate, Egypt. Asian journal of transfusion science. 2011;5(2):136-9.
Oncu S, Oncu S, Okyay P, Ertug S, Sakarya S. Prevalence and risk factors for HEV infection in pregnant women. Medical science monitor : international medical journal of experimental and clinical research. 2006;12(1):CR36-9.
Begum N, Devi SG, Husain SA, Ashok K, Kar P. Seroprevalence of subclinical HEV infection in pregnant women from north India: a hospital based study. The Indian journal of medical research. 2009;130(6):709-13.32.
Mamun Al M, Rahman S, Khan M, Karim F. HEV infection as an aetiologic factor for acute hepatitis: experience from a tertiary hospital in Bangladesh. Journal of health, population, and nutrition. 2009;27(1):14-9.
Machado A, Bordalo AA. Analysis of the bacterial community composition in acidic well water used for drinking in Guinea-Bissau, West Africa. Journal of environmental sciences. 2014;26(8):1605-14.
Scotto G, Martinelli D, Centra M, Querques M, Vittorio F, Delli Carri P, et al. Epidemiological and clinical features of HEV infection: a survey in the district of Foggia (Apulia, Southern Italy). Epidemiology and infection. 2014;142(2):287-94.
Galiana C, Fernandez-Barredo S, Perez-Gracia MT. [Prevalence of hepatitis E virus (HEV) and risk factors in pig workers and blood donors]. Enfermedades infecciosas y microbiologia clinica. 2010;28(9):602-7.
De Donno A, Chironna M, Craca R, Paiano A, Zizza A, Guido M, et al. [Anti-HEV seroprevalence in the area of Lecce]. Annali di igiene : medicina preventiva e di comunita. 2003;15(3):199-205.
khuroo MS, Teli MR Skidmore S, Sofi MA, Khuroo MI. Incidence and severity of viral hepatitis in pregnancy. Am J Med 1981;70:252-255.
Navaneethan, U., Al Mohajer, M., and Shata, M. Hepatitis E and Pregnancy Understanding the pathogenesis Liver Int. 2008; 28: 1190–1199.
Refbacks
- There are currently no refbacks.
